Lifestyle Resources
Health Resources
Medical Resources
Preventive Care
Resources
Help Center
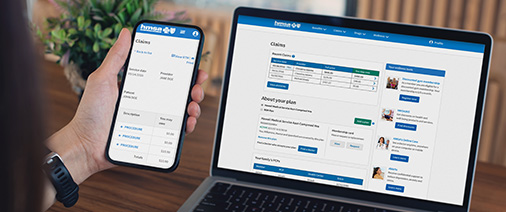
HMSA's My Account
Manage your plan online with HMSA’s My Account. My Account gives you convenient access to your health plan information.
Contact Us

HMSA Neighborhood Centers
Take control of your health care by getting answers to your questions from someone who knows. Our representatives can help you learn about your bill, make payments, check on a claim, explore well-being resources, or start a new plan.
- Health Plans More
- Well-being More
- Member Discounts More More
- Health Coaching
- HMSA's Online Care
- Maternal Health
- Quitting Tobacco & Cravings
- Telehealth
- Complex Case Management
- Condition Care Program
- Health and Well-being Support More More
- Post Hospital Discharge Program
- Pregnancy Support
- HMSA Diabetes Prevention Program
- Health Education Workshops
- Mental Health
- Help Center More
- Contact
- Employers
- Providers
- About More
- Careers More
- Media Center
- Awards and Scholarships More
- Sitemap
